Blood Cell Labeling 101
Variety of methods for the labeling of erythrocytes (red blood cells or RBC), leukocytes (white blood cells or WBC), and thrombocytes (platelet) have been established, employing either Tc-99m or In-111 as two of the most common radionuclides. Cardiovascular blood pool imaging, detection of GI bleeding and hemangioma, localization of inflammatory lesions, and thrombus detection are some of the applications in which blood cell labeling is utilized.
Erythrocytes

The methodology of RBC labeling is the most common of all the blood cell labeling to the point wherein several test kits are now available. In-111-oxine and Tc-99m-HMPAO (Hexamethylpropyleneamineoxime) are two of the most available test kits for non-specific techniques involving the use of lipophilic chelates through passive diffusion. Hence, the use of RBCs includes five major areas such as the following:
- measurement of the total RBC volume,
- measurement of the RBC survival time,
- identification of sites of RBC destruction,
- blood pool imaging studies, and
- selective spleen imaging
Thromboyctes
Platelets are extremely important physiologic mediator of clot formation and generation. According to a study (Coller et al., 1983), aside from In-111 and Tc-99m radionuclides such as I-123 and I-131 are also used for the same purpose. Labeling with I-123 and I-131 is equally effective in comparison with Tc-99m or In-111, since these isotopes of iodine yield an estimate of 80% binding capacity depending upon the reaction conditions.
Leukocytes
Studies on WBC labeling are still preliminary, although, promising researches (Locher et al., 1986) have been concluded that these blood components can locate abscesses and other inflammatory lesions. Tc-99m is the most preferred radionuclide with its 90% binding capacity although I-123 is more favored in cases of chronic lesions.
Facility Requirements for Blood Cell Labeling
Personnel and facility requirements are necessary to prevent operator exposure from the norms of radionuclides since the use of radionuclides is apparent in blood cell. In a document made by the Tygerberg Hospital and Stellenbosch University, several guidelines have been established for blood cell labeling.
A cleanroom with an ISO Class 7 or Grade C condition is required for blood cell labelling. Air monitoring for viable and non-viable particles should be performed regularly depending on the processes being handled inside a specific cleanroom. According to ISPE’s Sterile Manufacturing Facilities Guide, a cleanroom should maintain “a strict design regime, not only on the process area, but [also] on the interactions with surrounding areas and the movement of people, materials, and equipment, so as not to compromise the aseptic conditions.”
Laminar Air Flow (LAF) cabinets and isolators should maintain an ISO Class 5 environment. Regular checks for the filter integrity (using dioctyl phthalate), air velocity, airflow patterns (using smoke test), and particle count should be made monthly (maximum) or quarterly (maximum). It is advisable that HEPA filters should be replaced every 2-3 years, depending on the usage or if there are no pre-filters integrated. Ultraviolet (UV) lights should also be installed if possible. Centrifuges and laboratory refrigerators must be calibrated quarterly to monitor the wear and tear of parts.
Methods and protocols should be validated prior to first enactment and before the introduction for each new variation. Re-evaluation of the processes at regular intervals (every 6 months) is recommended to trace human or machine error.
The quality control (QC) process of blood cell labelling requires a four-step method which includes a) sterility testing, b) labeling efficiency, c) cell viability, and d) bio distribution. Out of these QC processes, sterility testing remains the priority since the maintenance of the purity of all the materials being handled will dictate the success of the entire blood cell labelling.
From conceptualization, planning, procurement, and installation, Esco is able to provide a comprehensive solution for cleanroom needs. Design consultation, site and workflow analysis, equipment selection, furniture design and material selection, shop drawings, lead time planning, product fabrication, installation, and commissioning services guarantees an ISO class environment of your choice.
Different classes of LAF and isolators suitable to the required process and budget requirements offer various degrees of containment while assuring a clean environment.
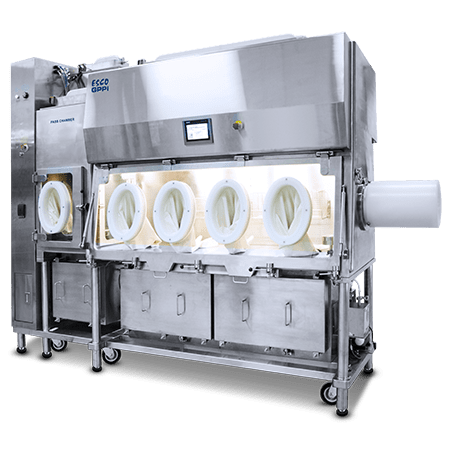
The Esco General Processing Platform Isolator (GPPI) is a highly adaptable, unidirectional laminar airflow isolator that can be used for sterility testing or other processes that require an ISO Class 5 (Grade A) aseptic environment. The GPPI’s advanced control system allows the operator to select either positive or negative chamber pressure as well as single pass or recirculating airflow patterns.

Aseptic Containment Isolator (ACTI) provides a premium handling of biopharmaceutical drug products and aseptic cell processing assuring an ISO Class 5 environment.





